Eye Conditions
Glaucoma
Glaucoma is the leading cause of preventable blindness in New Zealand, with an estimated 91,000 of Kiwis being affected by it. Approximately 50% of people with glaucoma don’t realise they have it – and yet 98% of the time it is treatable and manageable.
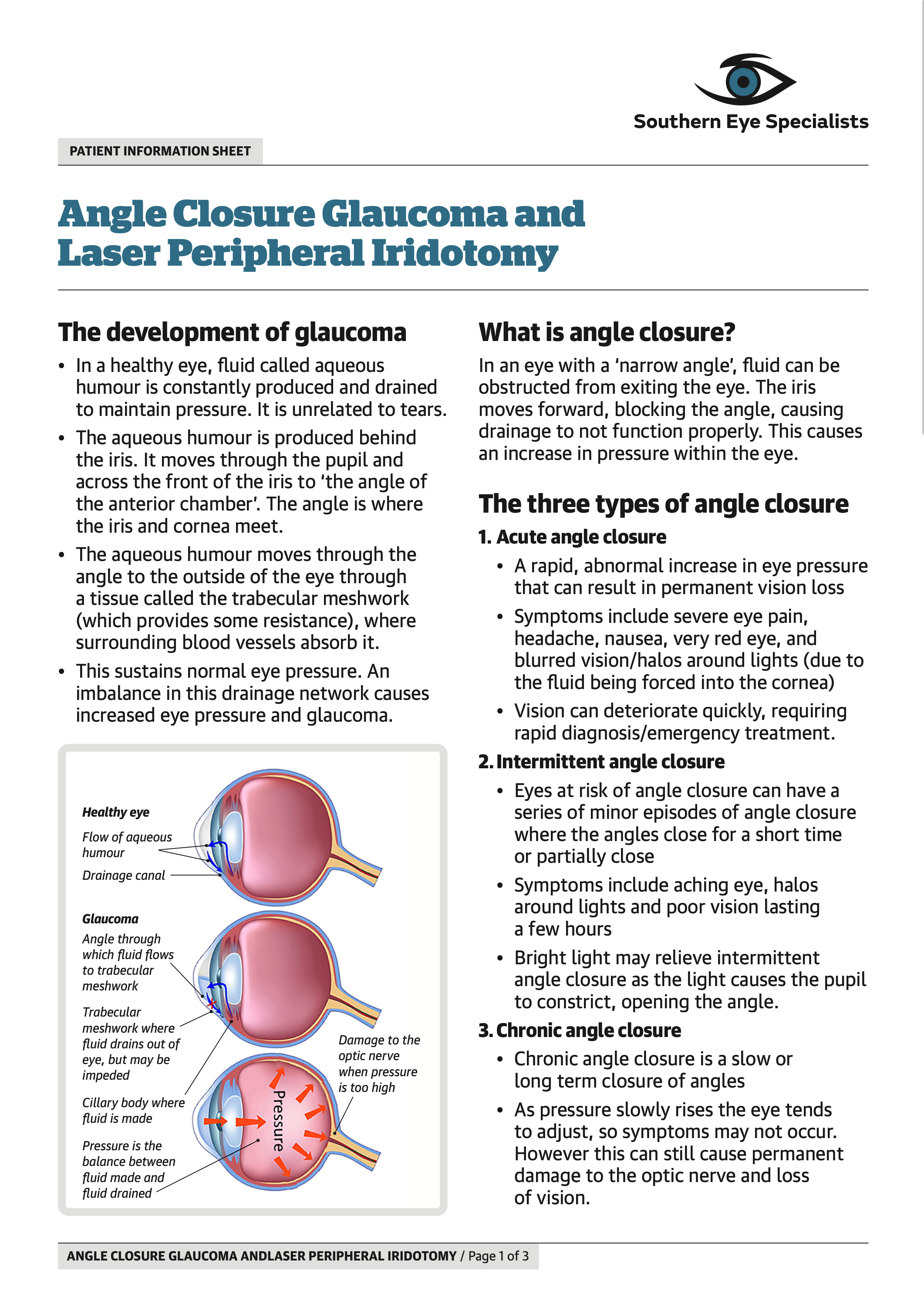
The imbalance between the in-flow and out-flow of fluid in the eye leads to the loss or degradation of peripheral vision and creates what is commonly known as ‘tunnel vision’. Lowering the pressure within the eye forms the basis for treating glaucoma.
While glaucoma is a serious and chronic disease, in most cases it can be well controlled. Early detection and regular monitoring by your eye specialist are key factors for maintaining normal vision.
Forms
There are two main forms of glaucoma. Open-angle glaucoma appears gradually and is more common. Closed-angle glaucoma can appear rapidly and requires immediate attention.
Cure
There is no definitive cure for glaucoma. However ongoing monitoring of eye pressure and a long-term treatment plan can prevent loss of vision.
Care
Care of glaucoma involves eye-drops, laser treatment and, in some instances, eye surgery.
Symptoms
50% of patients with glaucoma don’t know they have it as there are no symptoms early on. An examination by an eye specialist is the best way to pick up glaucoma when there are no symptoms.
FAQ’s
What exactly is glaucoma?
Glaucoma is the name given to a group of related diseases in which the eye’s optic nerve is damaged. The damage is slowly progressive, so is easy to go unnoticed – but once the optic nerve is damaged, it cannot be repaired. Glaucoma is typically caused by excessive eye pressure, which can be detected before any serious damage by regular check-ups.
How does glaucoma start?
A normal healthy optic nerve has about a million nerve fibres, which come from the retina (the seeing membrane at the back of the eye), and transfer the images to the brain for processing. When glaucoma develops, these nerve fibres start to die off and, if enough nerve tissue is lost, the vision starts to be affected.
Am I at risk of glaucoma due to my age?
Your eyes should be examined and tested for glaucoma regularly once you reach your 40s. From 40 to 50 eyesight should be tested every 5 years. From 50 to 60 this test should be 3 years, and from 60 onwards it should be every 2 years. If you have glaucoma risk factors you should be tested every 1-2 years after the age of 40.
What other risk factors are there for glaucoma?
If you have high eye pressure (intraocular pressure) there is a greater risk of developing glaucoma. Other risk factors include having a family history of glaucoma, certain medical conditions (diabetes, heart disease, high blood pressure and sickle cell anemia) and being extremely farsighted or nearsighted. As you get older there is also a greater risk of having glaucoma. If you have taken corticosteroid medications (especially eyedrops) for a long time, have had a significant eye injury, or after certain types of eye surgery, there may also be an increased risk.
Is there any type of glaucoma that needs early diagnosis?
Acute angle-closure glaucoma has symptoms that include a severe headache, eye pain, blurred vision and nausea. If these occur you should promptly go to Southern Eye Specialists or the nearest emergency department.
How do I get a glaucoma test?
Glaucoma is most commonly picked up during an appointment with an optometrist. Optometrists are well known for prescribing glasses, but during a comprehensive eye examination will also check for eye diseases, including a glaucoma. This examination will include measuring the eye pressure and possibly a visual field test.
What is the main method for treating glaucoma?
Prescribed eye drops are the best way of keeping Intraocular Pressure (IOP) down. This is a long-term treatment – if you stop using the medication your IOP will rise again and cause more irreversible damage. That’s why it’s very important to use your eye drops every day, and especially so on the days you visit your eye specialist – as they’ll need to determine whether your IOP is low enough with treatment.
How can I protect myself from glaucoma?
1. Get regular eye examinations – especially if you are over 40.
2. Check your family history as glaucoma will often run in families.
3. Look after your eyes. Wearing eye protection helps prevent injury, which can increase the chance of glaucoma.
4. Exercise. Regular exercise can reduce eye pressure, which reduces the risk of glaucoma.
5. If you are diagnosed with glaucoma, use the prescribed eye drops regularly and as directed by your ophthalmologist. These significantly diminish the chance that your high eye pressure will lead to glaucoma.
Can children get glaucoma?
Yes, they can but it is very rare. It may be present from birth or it can develop in their first few years. This is often cause by drainage blockages in the eye or an underlying medical condition.
How is glaucoma detected?
The damage glaucoma causes to the optic nerve can be detected in two ways, either by the way the nerve is working (such as problems with vision) or by abnormal changes in the structure of the nerve. To achieve this analysis we will generally use OCT scanning and Visual Field Test (VFT).
What is OCT scanning?
Optical Coherence Tomography (OCT) is an imaging test that provides us with a detailed view of the optic nerve head and retina. The OCT machine uses specific light waves to take a cross-section picture of the retina (similar to how an ultrasound uses sound waves).
What will happen in my OCT scan?
An OCT scan is painless and takes around 15 minutes. Dilating eye drops are administered first (which means you can’t drive for two to three hours afterwards). While the scan is taking place you will be asked to fix your vision on a bright light for short intervals. Following the scan you can view your test results with your eye specialists.
Why is this test so helpful?
In the past, deterioration was assessed by careful clinical examination, drawings or sometimes with digital photos. OCT can detect changes over time, and the scan can help determine how much your eye pressure needs to be lowered to halt further damage. This is why we recommend an initial baseline OCT scan for most cases of glaucoma, even if no further tests are done.
What is a Visual Field Test?
A Visual Field Test (VFT) is designed to assess the health of the peripheral vision. VFT is used to detect blind spots (scotomas) and other visual field defects that may indicate certain eye conditions. This test establishes a baseline that can then be used to assess any changes over time and guide the treatment of glaucoma.
Why is a VFT so important?
When glaucoma damages your eyes, it affects your peripheral vision first, almost always without you being aware of any symptoms. If glaucoma is not treated you may slowly and silently lose all peripheral vision. By the time central vision is affected and you notice a problem, the damage to the nerve fibres is already very severe, potentially resulting in irreversible blindness at the end stages. Because glaucoma is typically a slow and gradual disease, the VFT result can help assess damage and changes over time and establish the effectiveness of treatment.
What will happen in my VFT?
The Visual Field Test (VFT) takes around 10 minutes. It is in a quiet and darkened room, where a specialised technician will instruct you on what to do. One eye is tested while the other eye is covered. You are asked to look into a large dome-shaped machine with your eye focused on a central light. The light will vary in brightness and will appear off to the side of your vision. The test requires you to push a button whenever you see a light. The machine then analyses your results and provides the eye specialist with a map of your visual field.
How often will I have a VFT?
Your first VFT becomes your baseline. After this we will test you every 4 – 12 months, as instructed by your ophthalmologist. By comparing subsequent testing to your baseline result we can measure how well your treatment is working.
Where can I find out more about glaucoma?
Either speak to one of our nurses here, talk to your local optometrist or GP or go to Glaucoma NZ for further information.